To ice or not to ice an injury?
To ice or not to ice an injury?
This is probably one of the most common questions we get asked as a physio.
There seems to be a lot of confusion among the general population on when we should be using ice. To be honest, even among health professionals, there is a lot of confusion because the research is continuously changing.
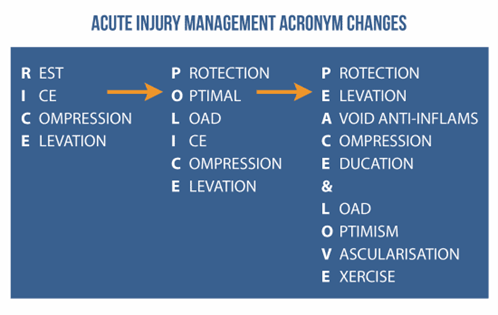
Most of us go by the acronym RICE (rest, ice, compression and elevation). This was first introduced in 1978 before ‘P’ was included for protection (PRICE). Since then, acute injury management protocols have been updated several times. 14 years later, POLICE (protection, optimal loading, ice, compression, elevation) replaced PRICE.
Ice was thought to minimise the inflammatory response in an attempt to accelerate healing. Furthermore, it’s now known that we need the inflammatory process to aid healing. Therefore, with the application of ice thought to delay the initiation of the inflammatory process, it’s use started to be significantly questioned.
Additionally, it was found that ‘Optimal Loading’ aids recovery through light loading exercises in the early phase (aka gentle range of motion and loading exercises). Subsequently, Rest (R) or a lack of movement is detrimental to recovery.
Because of this, in 2019 ice was retracted from the injury management protocol and replaced with PEACE (protection, elevation, avoid anti-inflammatories, compression, education and LOVE (load, optimism, re-vascularisation, exercise)
So with this new research, we still get many patients asking why does ice make my injury feel better then?
It’s widely accepted that ice helps to reduce pain by creating a numbing effect on injured tissues/areas. Ice alone doesn’t directly reduce swelling, which has been confirmed in several studies. In the circumstance where there is significant swelling (e.g – acute ankle sprains), ice may be a viable option, as the goal is not to necessarily prevent all swelling, but to limit the extent of it.
Too much or prolonged swelling is bad news - excessive swelling applies unwanted pressure on the tissues, restricts movement, can increase pain and decreases muscle function (e.g – acute ankle sprains).
In contrast, muscle tears often elicit less swelling and hence the application of ice is likely not going to be of benefit in the early stages (or at all) during injury management. It’s also worth noting that the topical application of ice has no influence over muscle temperature.
So should I be using ice?
Aside from acute trauma (less that 48 hours after injury), ice probably does not help beyond pain reduction. However, ice’s ability to reduce pain (numbing effect) makes it an effective and safe alternative in pain management.
Yes, sometimes ice is over-used and sometimes claimed to do things it probably doesn’t do. While there are some circumstances where ice may not be appropriate or helpful, ice IS supported in some situations.
For now, when there is significant amounts of swelling, ice in COMBINATION with gentle movement/range of motion exercises is encouraged.